
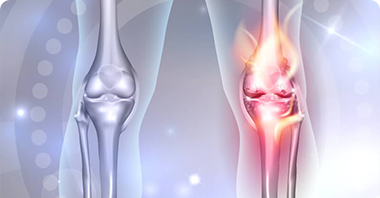
Replacing the missing or damaged meniscus with a meniscus from a cadaver donor or live amputee donor is called Meniscal transplant surgery. The surgery happens under anesthesia (General or Spinal or Epidural depending upon the patient’s anatomy). There are 2 wedge-shaped pieces of cartilage, placed on each side of the knee. These cartilages are called a “Meniscus.” They act as shock absorbers between shinbone and thighbone. They also help your bones move smoothly. Menisci protect the ends of thighbone and shinbone as they move together. Without this meniscus cushion, the ends of your thighbone and shinbone will rub against each other abnormally. This can lead to persistent knee pain. And in future, it may cause arthritis. Trauma & injury can cause damage to the meniscus. If more than 70% of the meniscus is damaged, then it needs to be surgically repaired. In such cases, Meniscal transplant surgery is the solution. A very small incision is done in the knee. Ortho Surgeons uses special instruments and cameras to access and evaluate the joint space between your thighbone and shinbone. And then, the surgeon surgically implants the donated meniscus into the joint space. Why “Meniscal transplant surgery”? Meniscal transplant surgery is appropriate and preferable if the patients’ meniscus was removed in a previous surgical procedure. Without a meniscus, the patient will eventually develop knee pain and joint arthritis. The meniscal transplant can provide significant relief in pain. It also helps in preventing joint arthritis. It’s a lesser invasive surgery than knee replacement surgery. But, in case the patient has already undergone meniscus removal and has knee arthritis, then this procedure might not help because the patient may have already done too much damage to his cartilage and bone. The procedure, like knee replacement surgery, might be more effective. Meniscal transplant surgery can do wonders, if the following applies to the patient: 1. He/she is younger than age 55. What happens after Surgery? Post-surgery, for a few weeks patient will have to wear a knee brace. He/she might also need to use crutches during this time. Surgeon will advise on how the patient should move the knee while he/she recovers. Physical therapy for a few months will also help the patient to maintain strength and range of motion. It takes several months before the individual returns to all his/her previous activities. The patient may have some fluid draining from the incision, which is normal. Consult your surgeon immediately if there is an increase in redness, swelling, or draining from the incision, or he/she has high fever, chills, or severe pain.
2. He/she has a large meniscus tear (around 70%) that is irreparable
3. He/she is missing more than half of meniscus.
4. He/she has a knee with normal alignment and stable ligaments.
5. He/she is not obese.
6. He/she has an unstable knee with persistent pain during an activity.
7. He/she has minimal arthritis.